







Facts all Ambulatory Surgery Centers Need to Know About Privileging

Regulations Your Ambulatory Surgery Center (ASC)Needs to Know About
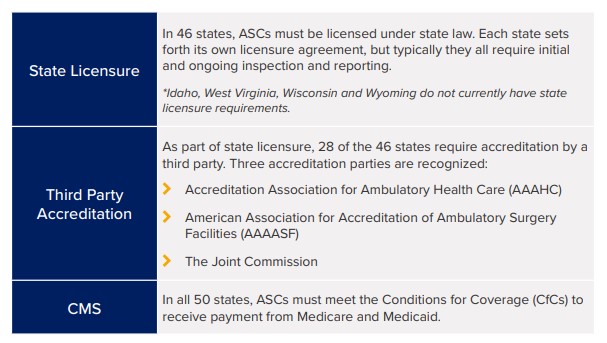
There are just under 10,000 ASCs in the U.S. Each one is required to have sometype of credentialing and privileging process in place. Some states are governedby state licensure, others require third party accreditation, and some must complywith both. In all 50 states, ASCs must meet the Centers for Medicare and MedicaidServices' (CMS) Conditions for Coverage (CfCs) to receive payment.
Current Stats:
- Only 60% of ASCs have met CMS' CfCs
- 930 ASCs are accredited by The Joint Commission
- 835 ASCs are accredited by the AAAHC
- 168 are accredited by the AAAASF
*Note: All accrediting organizations align their requirements with CMS' CfC which allows ASCsto receive "deemed status" with Medicare and Medicaid once they are accredited. This meansthat if you are accredited, for example, by The Joint Commission, you're also deemed to be incompliance with CMS' CfC.
All Accrediting Organizations Have Requirements in PlaceAround Credentialing and Privileging
Credentialing is an umbrella term used by many organizations to summarize theprocess of obtaining, verifying, and assessing the qualifications of a practitioner toprovide care or services in or for a health care organization. Privileging is a subsetof the credentialing process whereby a healthcare practitioner is authorized toprovide a specific scope of patient care services based on an evaluation of theindividual's credentials and performance. A privilege is defined as an advantage,right, or benefit that is not available to everyone, enjoyed by a relatively smallgroup of people, usually as a result of education and experience.
Credentialing and Privileging is a Top Challengefor Today's ASC
Credentialing and privileging are a heavy lift. If you're struggling with theseprocesses, you're not alone. A recent article published in Becker's ASC REVIEWnotes that The Joint Commission identified the following as the top threechallenges facing today's ASCs:
- Infection prevention and control
- Medical equipment disinfection
- Physician credentialing
Making sure that there is someone within your ASC who's maintaining yourcredentialing and privileging, reviewing records, securing evidence of currentlicensures, etc. and having a consistent process to do so are key to establishingand maintaining compliance.
The Journey Towards Clinical Competency
If you have any doubt at all about your ASC's ability to perform propercredentialing and privileging, your alarm bells should be ringing. In addition tobeing required by all accrediting organizations, credentialing and privileging isalso vital to patient safety and risk management. Your journey towards clinicalcompetency begins with gaining an understanding of the requirements in placeand implementing a process to enable you to deliver against those requirements.
When it comes to Privileging, all accrediting organizations require the following:
- Each ASC must have a governing body in place that is responsible for all privileging decisions. In some cases, this might be just one person, such as the owner of the ASC, but this individual must make all privileging decisions.
- All ASCs must have clearly defined credentialing and privileging policies and procedures that identify:
- The scope of the care your organization is providing
- Who is required to be credentialed and/or privileged to deliver those services
- The qualifications that a provider must possess to be privileged to practice those services in your facility, such as education, training, experience, board certification, etc.
- A process for verifying the qualifications required
- A process for making privileging decisions (Credentials Committee or other authorization pathway)
It's important to note that providers must be credentialed and privileged upon hireand every two years after that (except in Illinois, where it is required every threeyears). Reappointment requires data to demonstrate performance within yourASC, which will be used to support current competency.
The Role of a Credentials Verification Organization
There is a reason many hospitals have entire departments dedicatedto credentialing - it's a time-consuming process. In some cases,outsourcing the process may be your best option. ASCs can contractwith a credentials verification organization-commonly called a CVO-toobtain primary source verification. A CVO is defined as any organizationthat provides information on an individual's professional credentials.If your ASC bases a decision in part on information obtained from aCVO, it's important that you have a high level of confidence in thecompleteness, accuracy, and timeliness of the information provided.ASCs are not permitted to grant privileges based on the fact that aprovider might have privileges somewhere else. All ASCs must maketheir own decisions and these decisions need to be based upon datathat they have either collected themselves or have received from a CVO.
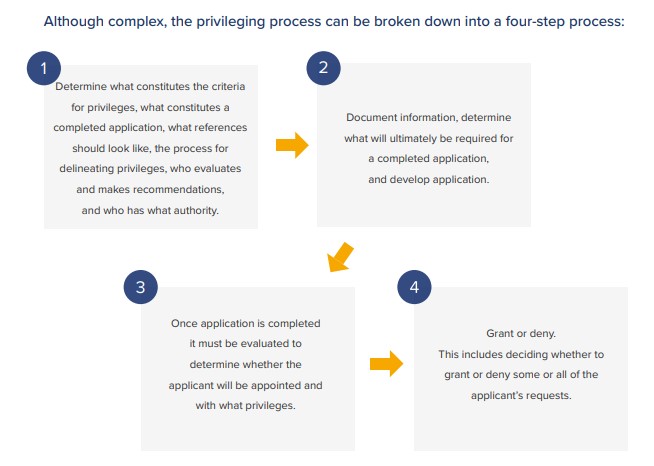
Process
With specific procedures in place, you'll gain a structure for all the important stepsin your privileging process, such as your exact decision-making methodology andhow you communicate throughout it. When mapping out your process, you mustconsider every element of clinical privileging including the:
- Delineation
- Request
- Recommendation
- Granting
- Monitoring
- Eventual lookup of provider privileges
Go Manual or Automate?
The credentialing and privileging process is complex, time-consuming, anddetail intensive. While implementing a manual process for your ASC is not out ofthe question, many organizations have found implementing a software solutionsaves time and increases quality. Pulling the content required for credentialingand privileging from disparate sources can be a tedious task. A software solutionthat comes with out of the box content - including privileging forms createdspecifically for your care setting and prebuilt credentialing and privilegingworkflows - will save you time and money. Software can also help prepare yourorganization for audits, securely store current/reliable provider information, andensure that all documents and accreditations are easy to find and remain secure.
It's important to realize that there is a lifecycle associated with the managementof your providers' competency and how you ensure clinical excellence at yoursurgery center. Software can help you answer questions like "how many" and"how well" and track other key performance metrics including clinical activity, general performance indicators, specialty-specific indicators, clinical case reviewresults, and benchmarks. This type of data analysis is virtually impossible withoutsome form of automation.
In Summary
As the government and payers scrutinize costs and push the shift to value-basedcare, outpatient surgery is expected to see an overall 11 percent increase from2017 to 2022. If you're operating an ASC - the time to get things right is NOW.
All ASCs are required by law to have some type of credentialing and privilegingprocess in place. Some states are governed by state licensure, others require thirdparty accreditation, and some must comply with both. All ASCs must meet CMS'Conditions for Coverage (CfCs) to receive payment. But compliance is only onepart of the equation. Setting up a first-rate credentialing and privileging processcan position you as an ASC of choice. An online electronic process that is easyto complete results in provider satisfaction and enables you to readily recruit andretain top talent. Top talent will improve your reputation and result in increasedbusiness. Implementing an efficient privileging process doesn't have to be hard -we're here to help!
