Achieve smarter, more efficient provider operations
Network by HealthStream® modernizes provider data, contracting, and credentialing with streamlined workflows and automation. Boost efficiency, reduce claims errors, cut costs, and eliminate rework while improving provider satisfaction and operational outcomes.

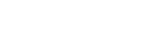
Eliminate data silos, enhance compliance
Ensure accuracy and compliance with Network's industry-leading provider management system. Automate updates, centralize data, and eliminate redundancies to enhance operational efficiency.





.avif)
Trusted. Certified. Secure.
Network by HealthStream, along with CredentialStream and related services, has achieved HITRUST Risk-based, 2-year Certification—the highest standard for healthcare data protection. This certification demonstrates our commitment to safeguarding sensitive provider data and exceeding compliance standards like HIPAA and GDPR. With zero data breaches and over 170 controls in place, HealthStream is a trusted partner in provider data security.
Built for the teams behind every trusted network
From credentialing to compliance, Network supports the people who ensure your provider data is accurate, timely, and audit-ready.

VP of Network Management
Ensure accurate, compliant provider networks

VP of Health Plan Operations
Streamline processes and reduce admin burden
Chief Compliance Officer
Mitigate risk with real-time monitoring

Department Managers
Manage shifts and staff quickly from one easy-to-use tool
b1daee0029444337892ed9aecbe4fd92.png)
Explore key features of Network
Discover what makes Network by HealthStream the right choice for health plans.
.svg)
Network—powered by hStream
Bring it all together with seamless access to the largest healthcare content marketplace, exclusive applications, specialized tools, and significant subscriber discounts.
Frequently Asked Questions
How can I integrate Network by HealthStream with my existing systems?
To learn more about how to seamlessly integrate Network by HealthStream with your existing systems, visit HealthStream's Developer Portal. There, you’ll find everything you need—APIs, detailed documentation, and expert support—to connect Network by HealthStream to your organization’s workflows. All integrations are powered by secure, enterprise-grade APIs with built-in identity management and monitoring.
What makes Network different from other provider data tools?
Network by HealthStream is purpose-built for payers with real-time credential monitoring, configurable workflows, and seamless integration with downstream systems like claims and directories.
Is Network compliant with NCQA and CMS standards?
Yes. Network supports compliance with National Committee for Quality Assurance (NCQA), Centers for Medicare and Medicaid Services (CMS), and other regulatory standards by automating credential checks, sanction monitoring, and audit documentation.
How long does implementation typically take?
Implementation timelines vary by organization size, but most payer clients are live within 9-12 months.
Can Network integrate with our existing systems?
Absolutely. Network offers flexible APIs and integration options to connect with your claims processing, provider directories, analytics tools, and more.
What types of provider data can Network manage?
Network handles licensure, sanctions, credentialing data, expirables, demographics, and delegation tracking—all in one centralized platform.
Who typically uses Network inside a payer organization?
Common users include credentialing teams, provider data managers, compliance officers, and network operations teams.
Get access to additional insights & resources
If you’re seeking a single source to manage:
- Network Relations
- Contracting
- Credentialing
- Provider Data








